Today we are pleased to feature five guest posts from students in Tom Ewing’s Virginia Tech Introduction to Data in Social Context class! This post is from Christian Averill, Robbie D’Amato, Nathan Gibson, and Jonathan Silbaugh.
During the nineteenth century, a widespread desire for a cure for tuberculosis prompted intense interest in any claims of a medical breakthrough in diagnosing and treating this disease. When German physician Robert Koch announced in 1882 that he had discovered that the cause of the disease was a bacillus known as M. Tuberculosis, his discovery was widely celebrated as a major medical breakthrough. Eight years later, however, his claims to have discovered a cure for tuberculosis aroused more substantive questions about the veracity of his claims as well as the methods, findings, and analysis advanced to support these claims. This post examines some of the evidence involved in this discussion with the goal of evaluating Koch’s claims relative to standard procedures used now to discover, test, and approve cures.
Koch’s discovery of a cure for tuberculosis was hailed immediately as “The Greatest Medical Discovery of the Present Century,” as indicated by the subtitle of a widely circulated publication, Prof. Koch’s Cure for Consumption, authored by Berlin physician Dr. H. Feller (Illustration 1). In this brochure, Feller praised Koch’s quest for “the noble structure of a scientifically supported method of cure for consumption,” (p. 14) which had the “enormous significance” of potentially eliminating a disease that causes more deaths worldwide than any other cause, leading to this summary statement by Feller: “The unsatisfactory medical treatment of consumption has given place to a deliberate well considered method of action, and therapeutic science will no longer fail in consequence of social inequalities; but all, whether rich or poor, will be participators in the blessings of this wonderful discovery.” (p. 49)
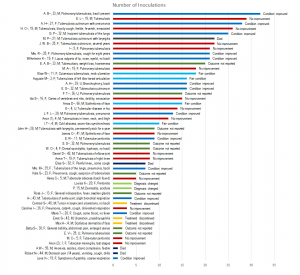
Yet a more complicated picture emerges when other physicians and researchers attempted to replicate Koch’s findings in their own laboratories and practices. One such effort to duplicate Koch’s findings, was recorded and reported by the American physician, A. Jacobi. The records for fifty patients treated with versions of Koch’s tuberculin were published, first in the journal Medical Record, and then in a separate volume, available from the Medical Heritage Library. The patients ranged in age from infants to the elderly, with about one-half between 20-50 years. The gender distribution was almost exactly even. Most of the patients were described as having pulmonary tuberculosis, although some had the disease in their bones or skin. Illustration 2 provides a visual analysis of the data collected by Dr. Jacobi and published in his report, as classified and recorded by our research team. The left column in the graph includes the identification of the patients by first name and initial (two were anonymous), gender, age, and a brief description of the patient’s disease. Patients covered in this study received as few as one inoculation and as many as thirty two inoculations over a period of many weeks. More than one-half of patients received ten or few inoculations; only about 10% of patients received 25 or more inoculations. This graph vividly illustrates how the effort to duplicate Dr. Koch’s experiments involved a wide range of treatments, with no apparent standardization. In some cases, it appears that treatments were discontinued because patients were diagnosed with another illness, while in other cases, the wishes of patients figured prominently in the treatment regime. The share of patients with negative outcomes (no improvement or died) was 38%, slightly higher than the 34% reporting positive outcomes (condition improved and fair condition), with another 28% recording neutral outcomes (outcome not reported, treatment discontinued, or diagnosis changed).
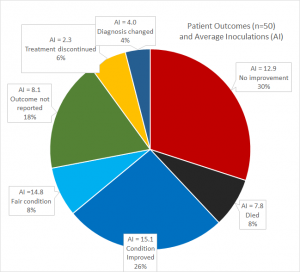
The most revealing interpretation suggested by this visualization of the data reported by Jacobi is the apparent lack of a causal relationship between the number of inoculations and the long term outcomes for patients. As shown in Illustration 3, patients recording more positive outcomes received, on average, more inoculations, certainly by comparison to those who died, whose diagnosis changed, or whose treatment was discontinued. Yet this data also reveals the relatively small gap in average inoculations between those showing improvement (an average of 15.1) and those showing no improvement (12.9), a gap of little more than two inoculations (a difference of just 15%) in treatment regimes that produced such diametrically opposed outcomes. Jacobi’s journal articles and book are revealing of the faith shared by researchers and the public in the process of medical discovery in the early 1890s.
Jacobi’s summary of the outcomes of his trials were cautiously optimistic, because he could compare the outcomes of those undergoing treatment with the usual “very discouraging” fate of those admitted to hospitals, particularly with pulmonary tuberculosis. While praising tuberculin as “a remedy of great power for good,” Jacobi also warned against viewing it as a miracle in ways that exaggerated its potential. Yet Jacobi concluded that tuberculin had done more than other remedies — apart from climatic treatment of pulmonary tuberculosis and surgical interference in cases of local tuberculosis — and thus he expressed gratitude to “great genii like Pasteur and Koch” who “enrich the world with new discoveries in the field of pathology and therapeutics,” yet even with these great scientists, “we must not look for infallibility.” (p. 43)
Under current testing standards, medical researchers today conduct highly regimented experiments following standard protocols, human subject guidelines, and control groups. A study such as Jacobi’s would most likely not meet standard practices common to the current scientific community. In Jacobi’s study, the data was easily measured and recorded. Current researchers, by contrast, use advancing medical technology to acquire higher quality data in greater quantity.
With the greater accessibility to high quality data, researchers today can make stronger conclusions about treatments. The data provided in Jacobi’s study did not clearly demonstrate the effects regarding the stability, safety, and effectiveness of this treatment for tuberculosis. The data produced by researchers such as Jacobi also reveal that the excitement for a TB cure caused premature conclusions about Koch’s treatment. Instead of testing to see the impact of the treatment, researchers were testing to see if his method was viable, leading to impulsive conclusions. Even though it is unclear that Koch’s treatment was viable as a cure, he still made an impact on the the cure for Tuberculosis.
References
Jacobi, A. (1891). Inoculations with Professor Koch’s “Tuberculin”. (New York: Trow’s Printing and Bookbinding Co., 1891). Articles originally published in Medical Record, February 29 and march 7, 1891. Digital version available from Medical Heritage Library and Internet Archive. Available from https://archive.org/details/101481837.nlm.nih.gov
Feller, H., Professor Koch’s Cure for Consumption (Tuberculosis) Popularly Explained (London: Ward, Lock, & Co., 1890). Digital version available from Medical Heritage Library and Internet Archive. Available from https://archive.org/details/39002011126829.med.yale.edu